Employee wellbeing programs have become table stakes for modern organizations, yet most companies are investing in solutions that miss the mark entirely. While Employee Assistance Programs (EAPs) remain the default corporate response to workforce mental health, the evidence tells a different story: the real drivers of employee wellbeing aren't found in crisis hotlines or counseling referrals—they're embedded in the daily behaviors, relationships, and management practices that define workplace culture.
At Happily.ai, we've spent years measuring what actually moves the needle on employee wellbeing. Using the World Health Organization's WHO-5 Well-Being Index—a clinically validated instrument translated into more than 30 languages and used in research studies worldwide (Topp et al., 2015)—we've discovered that organizations can achieve wellbeing improvements of up to 37% by focusing on something most companies overlook: the behavioral dynamics that shape how people experience work every day.
The EAP Problem: Why Traditional Approaches Fall Short
The inconvenient truth about Employee Assistance Programs is that almost nobody uses them. Research consistently shows that traditional EAPs have utilization rates between 2-10%, with the median hovering around 5.5% (National Business Group on Health, 2019). A study by Compton and McManus found that approximately 47% of employers reported employee utilization rates between just 2.1% and 8% (NAIC, 2015). In the UK, only 5% of employees access their EAP, largely because 60% of initial calls are redirected to self-help resources or external charities, eroding trust and follow-through (Meditopia, 2025).
The reasons for this underutilization are complex but well-documented. Research shows that employees often avoid EAPs due to stigma, lack of awareness, and fears that seeking help could negatively impact their careers (Reynolds & Lehman, 2003; Hu et al., 2012). Difficulty accessing services, lack of awareness, and unclear communication about confidentiality further discourage usage (Stone et al., 2023).
But here's the deeper problem: even when employees do use EAP services, the research on effectiveness is mixed. Some studies have found no reduction in individual stress after employees utilized these programs (Richmond et al., 2017). Others found no difference in presenteeism or absenteeism between groups with and without EAP interventions (Furukawa et al., 2012; Osilla et al., 2010). One study even found increased turnover intentions after certain types of EAP interventions (Caillier, 2017).
EAPs, by design, are reactive—they address problems after they've become severe enough that employees feel compelled to seek help. They function as tertiary interventions, treating existing diagnosed conditions rather than preventing problems from developing in the first place (Joyce et al., 2016). This approach misses an enormous opportunity: helping employees stay in the "green zone" rather than waiting until they've reached the "red zone" where external intervention becomes necessary.
A Different Philosophy: Wellbeing as Integral, Not Ancillary
What if wellbeing isn't a separate benefit to be outsourced to a third-party provider, but an integral component of how work gets done? This is the paradigm shift that separates effective workplace wellbeing strategies from the rest.
The U.S. Surgeon General's Framework for Workplace Mental Health & Well-Being identifies five essentials: Protection from Harm, Connection and Community, Work-Life Harmony, Mattering at Work, and Opportunity for Growth (HHS, 2022). Notice that none of these essentials can be delivered through an EAP. They require fundamental changes to workplace culture, management practices, and organizational behavior.
Mental Health America's 2024 workplace wellness research confirms this insight. Their findings show that workplace cultures built on trust and support improve employees' experiences of belonging, psychological safety, and empowerment—ultimately improving mental health and wellbeing (Mental Health America, 2024). The questions with the strongest correlation to overall workplace health scores were "My employer appreciates me for my contributions" and "I feel like I belong in my workplace."
This aligns with decades of organizational psychology research demonstrating that workplace culture significantly affects employees' happiness and job satisfaction (Srivastava & Dey, 2023). Supportive work environments that emphasize employee wellbeing lead to higher levels of job satisfaction and productivity, as well as better employee retention and organizational performance.
The Manager Effect: Your Biggest Wellbeing Lever
If there's one finding that should reshape how organizations think about employee wellbeing, it's this: managers have just as much impact on employees' mental health as their spouses—and more impact than their doctors or therapists (UKG, 2023). According to this landmark study of 3,400 people across 10 countries, 60% of employees worldwide say their job is the biggest factor influencing their mental health.
Gallup's research tells a similar story. When they tracked over 10,000 U.S. workers over six months, employees classified as engaged were five times more likely to report that their job had an "extremely positive impact" on their mental health compared to all other employees (Gallup, 2025). And what drives engagement? The quality of management.
Our own data at Happily.ai powerfully illustrates this manager effect. In an analysis of 869 managers, we found dramatic differences between the top 10% of people managers and everyone else:
Team Engagement (DEBI Score): Top 10% managers consistently achieve engagement scores in the "Good" range (65-80), while other managers often fall into the "Fair" or "Poor" zones (25-45).
Team Advocacy (eNPS): Teams led by exceptional managers show employee Net Promoter Scores ranging from +40 to +80—indicating strong workplace advocacy. Teams under other managers frequently score in negative territory, sometimes as low as -40.
Team Well-being (WHO-5): Perhaps most striking, teams with top managers report WHO-5 wellbeing scores averaging 75-80, while other teams score significantly lower, often in the 55-70 range.

What distinguishes these exceptional managers? They're more proactive and responsive. They address issues before they fester. They create environments where people feel psychologically safe raising concerns. They recognize that the things we think "shouldn't" be problems—the daily friction, miscommunications, and unresolved tensions—don't have to be problems we learn to live with. When solved in a timely way with people we actually enjoy solving problems with, these workplace dynamics transform from chronic stressors into opportunities for connection and growth.
Measuring What Matters: The WHO-5 Approach
Effective wellbeing improvement requires rigorous measurement. At Happily.ai, we use the WHO-5 Well-Being Index because it represents the gold standard for subjective wellbeing assessment. The scale has been found to have high clinimetric validity, can be used as an outcome measure in clinical trials, and serves as a sensitive screening tool for depression (Topp et al., 2015). Its five simple questions tap into the subjective wellbeing of respondents, focusing on positive mood, vitality, and general interest in life.
We administer the WHO-5 quarterly and establish baselines before program implementation, enabling us to track real change over time. This isn't about surveying people to death—it's about creating a meaningful feedback loop that helps organizations understand whether their culture investments are actually working.
The results have been remarkable. Across four organizations implementing our behavioral approach to culture and engagement, we documented the following WHO-5 improvements:
Company A: Mean wellbeing score increased from 45.7 to 62.7—a 37% improvement
Company B: Mean wellbeing score increased from 57.0 to 75.0—a 31% improvement
Company C: Mean wellbeing score increased from 63.7 to 75.9—a 19% improvement
Company D: Mean wellbeing score increased from 53.5 to 56.0—a 5% improvement
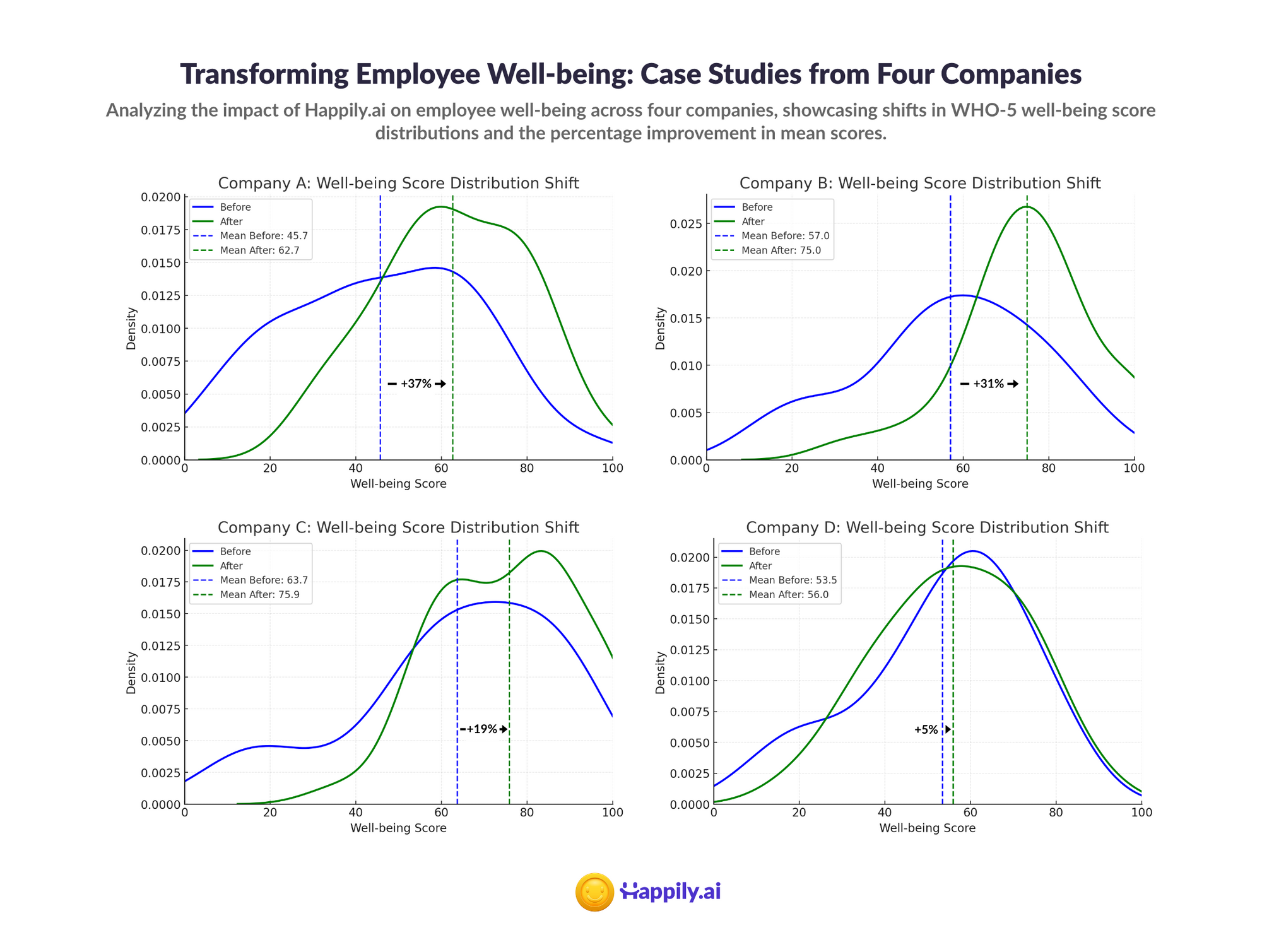
These aren't marginal gains. A 37% improvement in measured wellbeing represents a fundamental shift in how people experience work. And importantly, these improvements came not from adding more wellness benefits or EAP services, but from systematically improving the behavioral dynamics that shape daily work experience.
Culture as the Mechanism: Values, Belonging, and Relationships
What exactly are these "behavioral dynamics" that drive wellbeing? They're the behaviors that define how people do things in a workplace—behaviors centered around core values that help people feel a sense of belonging and create stronger bonds in relationships.
Research on workplace culture and mental health confirms that organizational culture significantly affects outcomes including stress, depression, and burnout (Srivastava & Dey, 2023). The U.S. Surgeon General's framework identifies social support and belonging as foundational human needs that must be met in the workplace for mental health to flourish (HHS, 2022). Having networks and relationships that offer physical and psychological help mitigates feelings of loneliness and isolation.
This is why surface-level wellness programs so often fail. They address symptoms without touching the underlying cultural dynamics. You can offer unlimited meditation app subscriptions, but if the workplace environment is characterized by distrust, poor communication, and unsupportive management, those meditation sessions won't move the needle on actual wellbeing.
The science of behavioral nudges offers a path forward. Rather than relying on employees to self-select into wellness programs, organizations can embed positive behaviors into the daily rhythm of work. Recognition becomes a regular practice rather than an annual event. Feedback flows continuously rather than being saved for performance reviews. Managers develop the habit of checking in on their people's wellbeing as naturally as they check in on projects.
Prevention Over Intervention: The Green-Yellow-Red Framework
Perhaps the most important paradigm shift in evidence-based wellbeing is moving from intervention to prevention. The public health model distinguishes between primary prevention (preventing problems from developing), secondary prevention (early detection and treatment), and tertiary prevention (managing existing conditions) (Joyce et al., 2016).
EAPs operate almost exclusively at the tertiary level—they're designed to help employees who have already developed significant mental health challenges. But research increasingly supports the value of primary and secondary prevention approaches in workplace settings (LaMontagne et al., 2014). Workplace interventions that prevent harm and promote the positive aspects of work have been shown to effectively optimize prevention while also managing mental health challenges when they do arise.
Think of it as a traffic light system:
Green Zone: Employees are thriving. They have the resources, relationships, and support they need. The goal here is maintenance and continued flourishing.
Yellow Zone: Warning signs are emerging. Energy is flagging, engagement is dropping, small frustrations are accumulating. This is where proactive intervention—a conversation with a manager, a shift in workload, a reconnection with purpose—can prevent deterioration.
Red Zone: Significant mental health challenges are present. Clinical intervention may be necessary. This is where EAPs have traditionally focused.
The problem with waiting for the red zone is that by the time someone reaches it, the damage to their wellbeing, their relationships, and their productivity has already accumulated. It's far more effective—and far more humane—to help people recognize when they're drifting from green to yellow and equip them with the tools and support to course-correct.
This requires measurement systems that can detect early warning signs, managers who are trained to have supportive conversations, and organizational cultures where seeking support isn't stigmatized. It requires, in short, treating wellbeing as a dynamic, ongoing practice rather than a crisis response capability.
The Business Case: Wellbeing Drives Performance
Some leaders still view employee wellbeing as a "nice to have"—important for employer branding perhaps, but separate from core business outcomes. The evidence strongly contradicts this view.
Gallup's extensive research has linked employee engagement to numerous organizational outcomes including profitability, productivity, customer service, retention, safety, and overall wellbeing (Gallup, 2025). The U.S. Surgeon General's report notes that chronic diseases and injuries in the U.S. workforce cost employers more than half a trillion dollars in lost productivity annually, and that organizations focusing on worker wellbeing see notable effects on organizational costs including reductions in absenteeism and health care claims (HHS, 2022).
The mechanism is straightforward: when people feel anxious or depressed, the quality, pace, and performance of their work declines (HHS, 2022). Workforce shortages are exacerbated by early exit and missed workdays due to health concerns, work-life conflicts, or burnout. Conversely, workplaces with engaged employees do a better job of keeping employees, satisfying customers, and being financially productive and profitable (Gallup, 2002).
In other words, workplace wellbeing and performance are not independent—they're complementary and dependent components of a financially and psychologically healthy workplace.
What This Means for Your Organization
If your current approach to employee wellbeing centers on providing EAP access and hoping employees use it, you're likely leaving significant value on the table—both in terms of actual employee health outcomes and business performance.
The evidence points toward a fundamentally different approach:
Invest in manager capability. Given that managers have more impact on mental health than therapists, developing your managers' ability to support, coach, and connect with their teams is probably your highest-leverage wellbeing investment. Training managers to create toxic-free workplaces and respond effectively to their teams should be a strategic priority.
Measure wellbeing directly. Use validated instruments like the WHO-5 to establish baselines and track progress. Leading indicators beat lagging ones—don't wait for turnover data to tell you something's wrong.
Build behavioral infrastructure. Embed practices that support wellbeing into daily work rhythms: regular check-ins, recognition, constructive feedback, and open communication about challenges and support needs.
Create cultures of belonging. Focus on the values, norms, and relationship dynamics that help people feel they're part of something meaningful. Culture isn't what you say on your website—it's how people experience work every day.
Shift from intervention to prevention. Help employees recognize early warning signs in themselves and others. Normalize conversations about mental health and remove the stigma from seeking support before reaching crisis point.
The Path Forward
At Happily.ai, improving employee health outcomes in a measurable way is a core part of our mission, along with making people measurably happier and more effective at work. We've seen what's possible when organizations move beyond the EAP paradigm and embrace a behavioral, culture-centered approach to wellbeing: 37% improvements in WHO-5 scores, dramatically higher engagement, and the creation of workplaces where people genuinely thrive.
This isn't about replacing EAPs entirely—crisis support services will always have their place. It's about recognizing that true wellbeing comes from addressing the daily workplace dynamics that shape how people feel about their work and their lives. It comes from managers who notice when something's off and know how to respond. It comes from cultures where people feel they belong and matter.
Employee wellbeing isn't a benefit to be administered. It's a human outcome to be cultivated—every day, in every interaction, through every behavioral choice that leaders and teams make together.
Ready to see how a behavioral approach to wellbeing could transform your organization? Learn more about Happily.ai and discover how we help organizations measurably improve the health, happiness, and effectiveness of their people.
References
Caillier, J. G. (2017). The impact of high-quality workplace relationships on organizational commitment: Evidence from a nationally representative survey. Review of Public Personnel Administration, 37(3), 374-395.
Furukawa, T., Horikoshi, M., Kawakami, N., et al. (2012). Telephone cognitive-behavioral therapy for subthreshold depression and presenteeism in workplace. Psychological Medicine, 42(10), 2079-2086.
Gallup. (2002). Business unit-level relationship between employee satisfaction, employee engagement, and business outcomes: A meta-analysis. Journal of Applied Psychology, 87(2), 268-279.
Gallup. (2025). The best management secrets for impacting employee mental health. Gallup Workplace Report.
HHS. (2022). The U.S. Surgeon General's Framework for Workplace Mental Health & Well-Being. U.S. Department of Health and Human Services.
Hu, Y., Stewart-Brown, S., Twigg, L., & Weich, S. (2012). Can the 12-item General Health Questionnaire be used to measure positive mental health? Psychological Medicine, 42(7), 1521-1531.
Joyce, S., Modini, M., Christensen, H., Mykletun, A., Bryant, R., Mitchell, P. B., & Harvey, S. B. (2016). Workplace interventions for common mental disorders: A systematic meta-review. Psychological Medicine, 46(4), 683-697.
LaMontagne, A., Martin, A., Page, K. M., Reavley, N. J., Noblet, A. J., Milner, A., Keegel, T. G., & Smith, P. M. (2014). Workplace mental health: Developing an integrated intervention approach. BMC Psychiatry, 14, 131.
Meditopia. (2025). EAP statistics and utilization rates in 2025. Meditopia for Work.
Mental Health America. (2024). Mind the workplace 2024: Healthy workplaces lead with trust and support.
NAIC. (2015). Mental health and employee assistance programs report. National Association of Insurance Commissioners.
National Business Group on Health. (2019). Quick survey findings: Employee assistance programs.
Osilla, K., Van Busum, K., Schnyer, C., Larkin, J. W., Eibner, C., & Mattke, S. (2010). Systematic review of the impact of worksite wellness programs. American Journal of Managed Care, 18(2), e68-e81.
Reynolds, G. S., & Lehman, W. E. (2003). Levels of substance use and willingness to use the employee assistance program. Journal of Behavioral Health Services & Research, 30(2), 238-248.
Richmond, M. K., Pampel, F. C., Wood, R. C., & Nunes, A. P. (2017). The impact of employee assistance services on workplace outcomes: Results of a prospective, quasi-experimental study. Journal of Occupational Health Psychology, 22(2), 170-179.
Srivastava, S., & Dey, B. (2023). A review on the impact of workplace culture on employee mental health and well-being. International Journal of Case Studies in Business, IT, and Education, 7(2), 291-317.
Stone, K. W., Kintziger, K. W., Jagger, M. A., & Horney, J. A. (2023). Understanding low utilization of employee assistance programs and time off by US public health workers during the COVID-19 pandemic. AJPM Focus, 2(2), 100082.
Topp, C. W., Østergaard, S. D., Søndergaard, S., & Bech, P. (2015). The WHO-5 Well-Being Index: A systematic review of the literature. Psychotherapy and Psychosomatics, 84(3), 167-176.
UKG. (2023). Mental health at work: Managers and money. The Workforce Institute at UKG.